Biomed Res Bull. 1(1):15-18.
doi: 10.34172/biomedrb.2023.05
Original Article
Enhancing the Expression of Interleukin-17 Level in Pemphigus Vulgaris Patients
Farshad Anguti 1  , Hesam Raziloo 2, Amir Mehdi Fununi 1, Salar Sereshteh 3, Mohadeseh Rajabpour 1, Ali Mohebbi 1, *
, Hesam Raziloo 2, Amir Mehdi Fununi 1, Salar Sereshteh 3, Mohadeseh Rajabpour 1, Ali Mohebbi 1, *
Author information:
1Department of Dermatology, Faculty of Medicine, Tabriz University of Medical Sciences, Tabriz, Iran
2Department of Internal Medicine, Faculty of Medicine, Tabriz University of Medical Sciences, Tabriz, Iran
3Department of Immunology, Faculty of Medicine, Tabriz University of Medical Sciences, Tabriz, Iran
Abstract
Background:
Pemphigus vulgaris is a chronic mucocutaneous condition and is the most common form of pemphigus. It produces blisters and erosions on the skin and mucous membranes. Pemphigus is a life-threatening autoimmune disease, and its prevalence has increased in recent years. Its etiology has not been well elucidated, but immunological factors have been reported to play a role.
Methods:
In the present cross-sectional case/control study, 18 patients with pemphigus vulgaris and 36 healthy subjects were included based on inclusion and exclusion criteria. Enzymelinked immunosorbent assay (ELISA) was used to determine interleukin (IL)-17 serum levels. Data were analyzed using descriptive parameters (means and standard deviations), and the Mann-Whitney U test was used to compare quantitative variables between the two groups by SPSS 16; furthermore, statistical significance was defined at P<0.05.
Results:
The means of IL-17 serum levels in patients with pemphigus and healthy subjects were 261.2±126 pg/mL and 35.7±11.6 pg/mL, respectively. Moreover, the Mann-Whitney U test revealed significantly higher serum levels of IL-17 in patients with pemphigus (P<0.05).
Conclusion:
Based on the results of the present study, the serum levels of IL-17 expression increased in pemphigus.
Keywords: Pemphigus vulgaris, Interleukin-17, Serum levels
Copyright and License Information
© 2023 The Author(s).
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Introduction
The term pemphigus refers to a group of potentially life-threatening autoimmune diseases. Pemphigus vulgaris is a chronic mucocutaneous condition and is the most common type of pemphigus, which results in blisters and erosions on the skin and mucous membranes.1 The susceptibility to the formation of autoantibodies leading to pemphigus is determined genetically; however, the mechanisms initiating the immune response are unknown.2 The disease most commonly occurs during the fifth and sixth decades of life. The predisposing mechanism for the formation of intra-epithelial lesions in pemphigus vulgaris is the binding of IgG antibodies to desmoglein I and desmoglein III, which strengthens cell-to-cell adhesion between epithelial cells. The loss of these adhesions due to a reaction between the antigen and antibody results in loosening and finally the destruction of connections between epithelial cells, desquamation, and formation of blisters.2,3 Pemphigus appears as a bulla with a thin membrane on the apparently normal skin or mucosa. Finally, the bulla ruptures denude a large area of skin. Nikolsky sign is used to diagnose pemphigus vulgaris. If pressure is applied on an intact blister, it will enlarge by expanding on the surface of the apparently normal skin, or if an area of skin without a blister is directly pressed, a blister will form in this area because the superficial layer of the skin moves away from the basal layer.4-6
Some patients (80‒90%) with pemphigus vulgaris have oral manifestations, and in 60% of the cases, the oral manifestations are the first signs of the condition. The bullae in the oral cavity break rapidly, and intact bullae are rarely found in the oral cavity. The majority of these lesions are seen in the oral cavity as shallow ulcers. Bullae take several weeks to develop and involve a wide area of the oral cavity. The first lesions appear on the buccal mucosa, which is attributed to traumas resulting from masticatory function. The palate and gingival tissues are also involved.7
Pemphigus vulgaris is diagnosed by biopsy which should be taken from intact bullae during the first 24 hours after their appearance. Biopsies are taken from the margins of the lesion so that acantholysis of the basal layer would be seen in the biopsy. If a biopsy sample is taken from the center of the lesion, an unspecific appearance will be observed. Sometimes, it is necessary to take several biopsies, and sometimes, a new lesion is induced by Nikolsky signs, and a biopsy is taken from the same area.8 Early diagnosis of this condition plays a great role in the control of lesions. Recently, the role of interleukin (IL)-17, which is secreted by Th17 cells, has been shown in a large number of autoimmune diseases, including rheumatoid arthritis, psoriasis, multiple sclerosis (MS), and bowel inflammatory diseases.9,10 Toto et al carried out a review study to evaluate IL-17 family elements and their role in inflammation, reporting that the family has 6 members from IL-17A to IL-17F.11 IL-17A is predominantly released by memory T cells and stimulates innate immunity and host defense. IL-17A and IL-17F recruit neutrophils through the induction of granulocytes and CXC chemokines and sustain their presence in the involved area. The release of IL-17A and IL-17F by T lymphocytes is regulated by IL-23, independent of the activity of the T-cell receptor.12-14 Based on the available evidence, an increase in the concentration of IL-17 family members has an active role in inflammatory diseases, autoimmune conditions, and cancer. Therefore, IL-17 family members and their receptors will become potential targets in pharmacotherapy. At present, based on the bulk of the empirical evidence, the activity of IL-17 family members is mediated through the release of proinflammatory cytokines in tissues. In a study carried out in the Department of Oral Medicine, Tabriz Faculty of Dentistry, the serum levels of IL-17 in patients with oral lichen planus were significantly higher than those in healthy subjects.5
Materials and Methods
In the present cross-sectional case/control study, the subjects consisted of 36 healthy individuals and 18 patients with oral pemphigus vulgaris based on clinico-pathological diagnosis, referring to Sina Hospital, Tabriz University of Medical Sciences.
Sampling Procedure
In the present study, a simple sampling technique was used due to the limited number of subjects. Healthy subjects were selected based on a simple random sampling technique from healthy subjects referring to Tabriz Faculty of Dentistry to receive a therapeutic procedure. Age and gender were matched in the two case and control groups.
Inclusion Criteria
The inclusion criteria included affliction with oral pemphigus vulgaris based on clinico-pathological manifestations and an age range of 18‒60 years.
Exclusion Criteria
Exclusion criteria were allergy, asthma, congenital and acquired defects of the immune system, (e.g., AIDS), chemotherapy, injection drug abuse, pregnancy, congenital pemphigus, drug-induced pemphigus, any contraindication for taking biopsies from the lesions, and a lack of consent to take part in the study.
Procedural Steps
A medical history was taken from all the patients, and a primary questionnaire was completed. After a biopsy was taken, a blood sample was taken from each patient in order to determine IL-17 serum levels using the IL-17 kit from eBioscience Company. At first, the anti-IL-17 antibody was coated in its special plate and then added to the patient’s serum. After incubation for a specific period of time, the second antibody, labeled with biotin, was added, incubated again, and rinsed; afterward, the enzymatic substrate was added. The color change which indicates the concentration of the serum cytokine was evaluated, and the concentration of the IL was determined based on a graph of standard concentrations.
Data Analysis
Data were analyzed by descriptive statistics (means and standard deviations), and the Mann-Whitney U test was used to compare quantitative variables between the two groups via SPSS 16. Further, statistical significance was defined at P < 0.05.
Results
In the present study, 18 patients with pemphigus vulgaris and 36 healthy subjects were evaluated. In both groups, 50% of the subjects were male and 50% were female. The mean age of the subjects in the case group was 33.2 years, with minimum and maximum ages of 22 and 42 years, respectively. The mean age of the subjects in the control group was 32.4 years, with minimum and maximum ages of 23 and 43 years, respectively. Moreover, the overall mean age of the subjects was 32.7 years, with minimum and maximum ages of 22 and 43 years, respectively (Table 1). Furthermore, there were no statistically significant differences in mean ages between the two groups (P > 0.05).
Table 1.
Means and standard deviations of the ages of subjects in the two groups under study
|
Group
|
Mean (±Standard deviation)
|
Minimum
|
Maximum
|
| Case (n = 18) |
33.2 ( ± 5) |
22 |
42 |
| Control (n = 36) |
32.4 ( ± 5.3) |
23 |
43 |
The mean serum levels of IL-17 in pemphigus patients and healthy subjects were 261.2 ± 126 and 35.7 ± 11.6 pg/mL, respectively. Further, the Mann-Whitney U test indicated significantly higher IL-17 serum levels in patients with pemphigus compared to healthy individuals (P < 0.05). Table 2 presents IL-17 serum levels in the case and control groups.
Table 2.
Means and standard deviations, and minimum and maximum serum levels of IL-17 in the case and control groups
|
Group
|
Mean (±Standard deviation)
|
Minimum
|
Maximum
|
| Case (n = 18) |
261.2 ( ± 126) |
83.3 |
567.3 |
| Control (n = 36) |
35.7 ( ± 11.6) |
20 |
61 |
Generally, it was concluded that in the subjects in the present study, the mean IL-17 serum levels were higher in patients with pemphigus compared to those in healthy subjects.
The Kolmogorov-Smirnov test was used to evaluate the normal distribution of IL-17 serum levels, revealing that the variable was not normally distributed (Kolmogorov-Smirnov Z = 2.32, P = 0.00). Therefore, the data were non-parametric; accordingly, the Mann-Whitney U test was used to compare IL-17 serum levels in healthy individuals and patients with pemphigus vulgaris at a significance level of P < 0.05. The null hypothesis of the study predicted no significant differences in the mean serum levels of IL-17 between healthy subjects and patients with pemphigus vulgaris. Based on the results of the Mann-Whitney U test, the null hypothesis was refuted, and it was found that the mean IL-17 serum levels in patients with pemphigus vulgaris were significantly higher than those in healthy individuals (P = 0.00) at a 95% confidence interval, as depicted in Figures 1A and 1B.
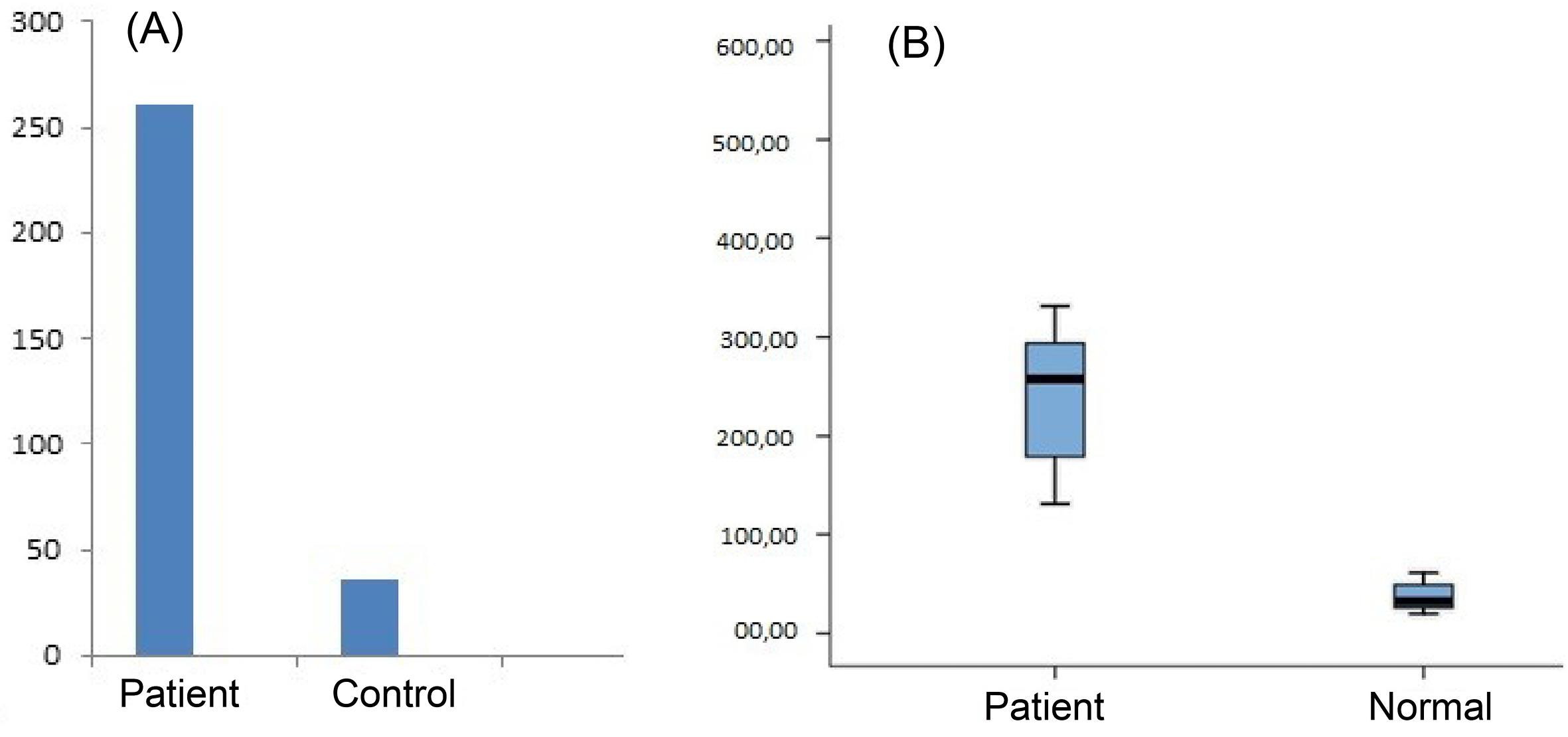
Figure 1.
(A) The box plot of il-17 serum levels in the two groups. (B) The means of il-17 serum levels (pg/mL) in the case and control
.
(A) The box plot of il-17 serum levels in the two groups. (B) The means of il-17 serum levels (pg/mL) in the case and control
Discussion
Pemphigus is an autoimmune disease in which due to unknown reasons antibodies are activated against glycoproteins on the surface of epithelial cells such as desmoglein I and III, which are components making up desmosomes. The most common type of this condition is pemphigus vulgaris. Oral lesions are the first signs in the majority of cases, and it is extremely difficult to treat them. When the anti-desmoglein antibody binds to its target antigen, the adhesive function of desmosomes is lost, leading to acantholysis.15 However, various studies worldwide have indicated that proinflammatory cytokines such as tumor necrosis factor α, IL-10, and IL-1α have an important role in acantholysis.16
Nguyen et al carried out a human/animal study and reported that there was an increased response of the Th17/IL-23 immune system pathway in mice and humans with Sjögren’s syndrome, which was associated with an increase in IL-17 and IL-23 levels during the active phase of the disease.12 Costa et al evaluated serum levels of several cytokines in patients with autoimmune diseases. The results showed an increase in serum levels of IL-17 and the target tissues of various autoimmune diseases.13,14 Studies reported that Th17 cells have a role in inflammatory conditions and recruit white blood cells to the infective and injury sites, mounting a strong immunologic response.15 Hofstetter et al evaluated the role of IL-17 in patients with MS and reported that Th17 cells can be considered effector T cells in autoimmune diseases of the central nervous system, similar to the role of IL-17 in other autoimmune diseases, including oral lichen planus. They concluded that specific and targeted treatment strategies to neutralize IL-17 or inhibit Th17 cells specific for central nervous system autoantigens might be considered immunotherapy goals.16
Yetkin et al evaluated IL11/IL-17 ratio in the gingival crevicular fluid in 40 patients with periodontitis and reported an increase in IL-17 levels with an increase in pocket depth and bone loss. Consistent with the results of the present study, they also demonstrated an increase in IL-17 levels as an immunopathologic factor in patients with pemphigus vulgaris.17 Moreover, Vernal et al reported higher concentrations of IL-17 in the gingival crevicular fluid in patients with chronic periodontitis compared to healthy controls, and consistent with the results of the present study, they found a higher concentration of IL-17 in inflammatory conditions.18 Mesquita et al suggested further studies on the basic biology of Th17 cells, including the background regulation of the epigenetic locus of IL-17 and other proinflammatory cytokines of this lymphocytic group.19 Due to the pleiotropic effects of IL-17 on fibroblasts, keratinocytes, endothelial cells, neutrophils, and memory T cells, it appears that Th17 cells have a major role in inducing tissue inflammation and autoimmunity. Classically, autoimmune diseases are considered Th1-dependent diseases which include MS, or Th1/Th2-dependent diseases which involve bowel inflammatory conditions, and bullous diseases such as pemphigus vulgaris. However, recent evidence indicates a major role for Th17 cells in the pathogenesis of these diseases. In addition, these findings demonstrate the therapeutic potential of the Th17/IL-17 pathway.20
To the best of our knowledge, no studies are available to document a decrease in IL-17 levels in autoimmune diseases, which would be in opposition to the results of the present study. The present study aimed not to evaluate the reasons for an increase in IL-17 levels. However, based on the results of previous studies and by ignoring the role of confounding factors, with regard to the role of IL-17 in pemphigus vulgaris, it can be concluded that IL-17 can play a role in the etiology of this condition through the production of large amounts of proinflammatory cytokines19 since there is an increase in IL-17 levels in inflammatory diseases, since pemphigus vulgaris is an inflammatory disease. On the other hand, the integrity of mucosa is lost in pemphigus vulgaris, and secondary infections might occur, which in turn might result in an increase in IL-17 levels. Therefore, an increase in IL-17 levels in pemphigus vulgaris might be attributed to the presence of inflammation or to superimposition of secondary infections. The present study is one of the few studies devoted to the role of IL-17 in the etiology of pemphigus vulgaris, and its results might contribute to determining the severity of inflammation and follow-up of the treatment course in addition to immunotherapy based on neutralizing IL-17 and IL-23 through inhibiting IL-23/Th17 pathway and neutralizing IL-12 through inhibiting Th1/IFN-8 pathway.
Conclusion
Based on the results of the present study, there was an increase in serum levels of IL-17 in patients with pemphigus vulgaris, which might indicate the inflammatory properties of this cytokine and its role in inducing the production of other proinflammatory cytokines.
Authors’ Contribution
Conceptualization: Farshad Anguti, Hesam Raziloo.
Data Curation: Amir Mehdi Fununi, Salar Sereshteh.
Formal Analysis: Mohadeseh Rajabpour, Ali Mohebbi.
Funding Acquisition: Ali Mohebbi.
Investigation: Ali Mohebbi.
Methodology: Mohaddeseh Rajabpour.
Project Administration: Alimohebbi.
Resources: Farshad Anguti.
Supervision: Ali Mohebbi.
Validation: Ali Mohebbi.
Visualization: Farshad Anguti.
Writing — Original Draft: Hesam Raziloo.
Writing — Review & Editing: Ali Mohebbi.
Competing Interests
None to be declared.
Ethical Approval
The study was approved by the Ethics Committee of Tabriz University of Medical Sciences (IR.TBZMED.REC.1401.863).
References
- Greenberg MS, Glick M, Jonathan A. Ulcerative, vesicular and bullous lesions. In: Burket’s Oral Medicine. Wiley; 2008.
- Chi W, Yang P, Zhu X, Wang Y, Chen L, Huang X. Production of interleukin-17 in Behcet’s disease is inhibited by cyclosporin A. Mol Vis 2010; 16:880-6. [ Google Scholar]
- Miossec P. IL-17 and Th17 cells in human inflammatory diseases. Microbes Infect 2009; 11(5):625-30. doi: 10.1016/j.micinf.2009.04.003 [Crossref] [ Google Scholar]
- Kolls JK, Lindén A. Interleukin-17 family members and inflammation. Immunity 2004; 21(4):467-76. doi: 10.1016/j.immuni.2004.08.018 [Crossref] [ Google Scholar]
- Pouralibaba F, Pakdel F. Evaluation of IL-17 Serum Levels in Patients with Oral Lichen Planus [dissertation]. Tabriz, Iran: Faculty of Dentistry, Tabriz University of Medical Sciences; 2010.
- Neville BW, Damm DD, Carl A, Chi A. Oral and Maxillofacial Pathology. Saunders; 2009.
- Bhol KC, Desai A, Kumari S, Colon JE, Ahmed AR. Pemphigus vulgaris: the role of IL-1 and IL-1 receptor antagonist in pathogenesis and effects of intravenous immunoglobulin on their production. Clin Immunol 2001; 100(2):172-80. doi: 10.1006/clim.2001.5061 [Crossref] [ Google Scholar]
- Feliciani C, Gupta AK, Sauder DN. Keratinocytes and cytokine/growth factors. Crit Rev Oral Biol Med 1996; 7(4):300-18. doi: 10.1177/10454411960070040101 [Crossref] [ Google Scholar]
- Feliciani C, Toto P, Amerio P. In vitro C3 mRNA expression in pemphigus vulgaris: complement activation is increased by IL-1alpha and TNF-alpha. J Cutan Med Surg 1999; 3(3):140-4. doi: 10.1177/120347549900300306 [Crossref] [ Google Scholar]
- Feliciani C, Toto P, Wang B, Sauder DN, Amerio P, Tulli A. Urokinase plasminogen activator mRNA is induced by IL-1alpha and TNF-alpha in in vitro acantholysis. Exp Dermatol 2003; 12(4):466-71. doi: 10.1034/j.1600-0625.2002.120415.x [Crossref] [ Google Scholar]
- Toto P, Feliciani C, Amerio P, Suzuki H, Wang B, Shivji GM. Immune modulation in pemphigus vulgaris: role of CD28 and IL-10. J Immunol 2000; 164(1):522-9. doi: 10.4049/jimmunol.164.1.522 [Crossref] [ Google Scholar]
- Nguyen CQ, Hu MH, Li Y, Stewart C, Peck AB. Salivary gland tissue expression of interleukin-23 and interleukin-17 in Sjögren’s syndrome: findings in humans and mice. Arthritis Rheum 2008; 58(3):734-43. doi: 10.1002/art.23214 [Crossref] [ Google Scholar]
- Costa VS, Mattana TC, da Silva ME. Unregulated IL-23/IL-17 immune response in autoimmune diseases. Diabetes Res Clin Pract 2010; 88(3):222-6. doi: 10.1016/j.diabres.2010.03.014 [Crossref] [ Google Scholar]
- Fouser LA, Wright JF, Dunussi-Joannopoulos K, Collins M. Th17 cytokines and their emerging roles in inflammation and autoimmunity. Immunol Rev 2008; 226:87-102. doi: 10.1111/j.1600-065X.2008.00712.x [Crossref] [ Google Scholar]
- Miossec P. IL-17 and Th17 cells in human inflammatory diseases. Microbes Infect 2009; 11(5):625-30. doi: 10.1016/j.micinf.2009.04.003 [Crossref] [ Google Scholar]
- Hofstetter H, Gold R, Hartung HP. Th17 cells in MS and experimental autoimmune encephalomyelitis. Int MS J 2009; 16(1):12-8. [ Google Scholar]
- Yetkin Ay Z, Sütçü R, Uskun E, Bozkurt FY, Berker E. The impact of the IL-11:IL-17 ratio on the chronic periodontitis pathogenesis: a preliminary report. Oral Dis 2009; 15(1):93-9. doi: 10.1111/j.1601-0825.2008.01497.x [Crossref] [ Google Scholar]
- Vernal R, Dutzan N, Chaparro A, Puente J, Antonieta Valenzuela M, Gamonal J. Levels of interleukin-17 in gingival crevicular fluid and in supernatants of cellular cultures of gingival tissue from patients with chronic periodontitis. J Clin Periodontol 2005; 32(4):383-9. doi: 10.1111/j.1600-051X.2005.00684.x [Crossref] [ Google Scholar]
- Mesquita D Jr, Cruvinel WM, Câmara NO, Kállas EG, Andrade LE. Autoimmune diseases in the TH17 era. Braz J Med Biol Res 2009; 42(6):476-86. doi: 10.1590/s0100-879x2009000600002 [Crossref] [ Google Scholar]
- Chiricozzi A, Zhang S, Dattola A, Cannizzaro MV, Gabellini M, Chimenti S. New insights into the pathogenesis of cutaneous autoimmune disorders. J Biol Regul Homeost Agents 2012; 26(2):165-70. [ Google Scholar]