Biomed Res Bull. 1(2):84-86.
doi: 10.34172/biomedrb.2023.15
Case Report
Classic Kaposi Sarcoma: An Unusual Presentation in an HIV-Negative Man
Mahsa Eslami 1  , Sanaz Alizadeh 2, Faezeh Alavi 1, Sina Safari 1, 2, *
, Sanaz Alizadeh 2, Faezeh Alavi 1, Sina Safari 1, 2, * 
Author information:
1Immunology Research Center, Tabriz University of Medical Sciences, Tabriz, Iran
2Department of Dermatology, Faculty of Medicine, Tabriz University of Medical Sciences, Tabriz, Iran
Abstract
Kaposi sarcoma (KS) is a type of cancer that develops in blood vessels of the mouth, lymph nodes, and lungs. Our case report is about a 66-year-old man with purple patches and plaques, as well as nodules distributed in the legs and arms. Biopsy of the skin lesions showed angiomatous proliferation of small vessels with mild perivascular lymphocytic infiltration with plasma cells. We started chemotherapy for this disseminated form of Kaposi sarcoma.
Keywords: KS, HIV, Case
Copyright and License Information
© 2023 The Author(s).
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Introduction
Kaposi sarcoma (KS) is a spindle-cell tumor caused by human herpesvirus 8 (HHV-8).1 Generally, this cancer occurs in HIV-positive people because their immune system is weakened. Lesions of KS usually occur in the skin, oral mucosa, lymph nodes, and visceral organs. Visceral disease may occasionally precede cutaneous manifestations.2,3 The classic form of visceral disease has a more indolent course than AIDS-related KS, which progresses over 10-15 years or more with highly gradual enlargement of cutaneous lesions.4 CD4 lymphocyte counts and plasma HIV viral-load studies should be performed in patients with HIV infection. Chest radiographic findings in patients with KS are variable and nonspecific. These findings may include diffuse reticulonodular infiltrates, interstitial infiltrates, pleural effusions, hilar or mediastinal lymphadenopathy, or an isolated pulmonary nodule.5-7 Thallium and gallium scans may help differentiate pulmonary KS from infection. Pulmonary KS lesions typically display intense thallium uptake but no gallium uptake, whereas the infection is often gallium-avid and thallium-negative.8 Immunomodulation with interferon-α has clinical activity in KS, which may be mediated by its antiangiogenic, antiviral, and immunomodulatory properties.9 In the pathology diagnosis, it is not diagnosed as sarcoma but a tumor arising from transformed cells with mesenchymal origin. HHV-8, also known as KS-associated herpesvirus (KSHV), is the primary factor in the pathogenesis of KS. KSHV proteins are uniformly detected in KS cancer cells.10-12 This discovery spawned a renewed interest in the disease, resulting in a significant amount of research to explain the relationship between HHV-8 and the uncontrolled vascular proliferation found in KS. KS lesions contain tumor cells with a characteristically abnormal elongated shape, called spindle cells. The most typical feature of KS is the presence of spindle cells forming slits containing red blood cells.13-19
Case Report
Here, we report a case of a 66-years-old man who referred to dermatology clinic of Sina hospital in Tabriz, Iran, with progressive skin lesions, including purple patches, plaques, and nodules distributed on the legs, trunk, arms, and hands from 3 years ago (Figure 1).
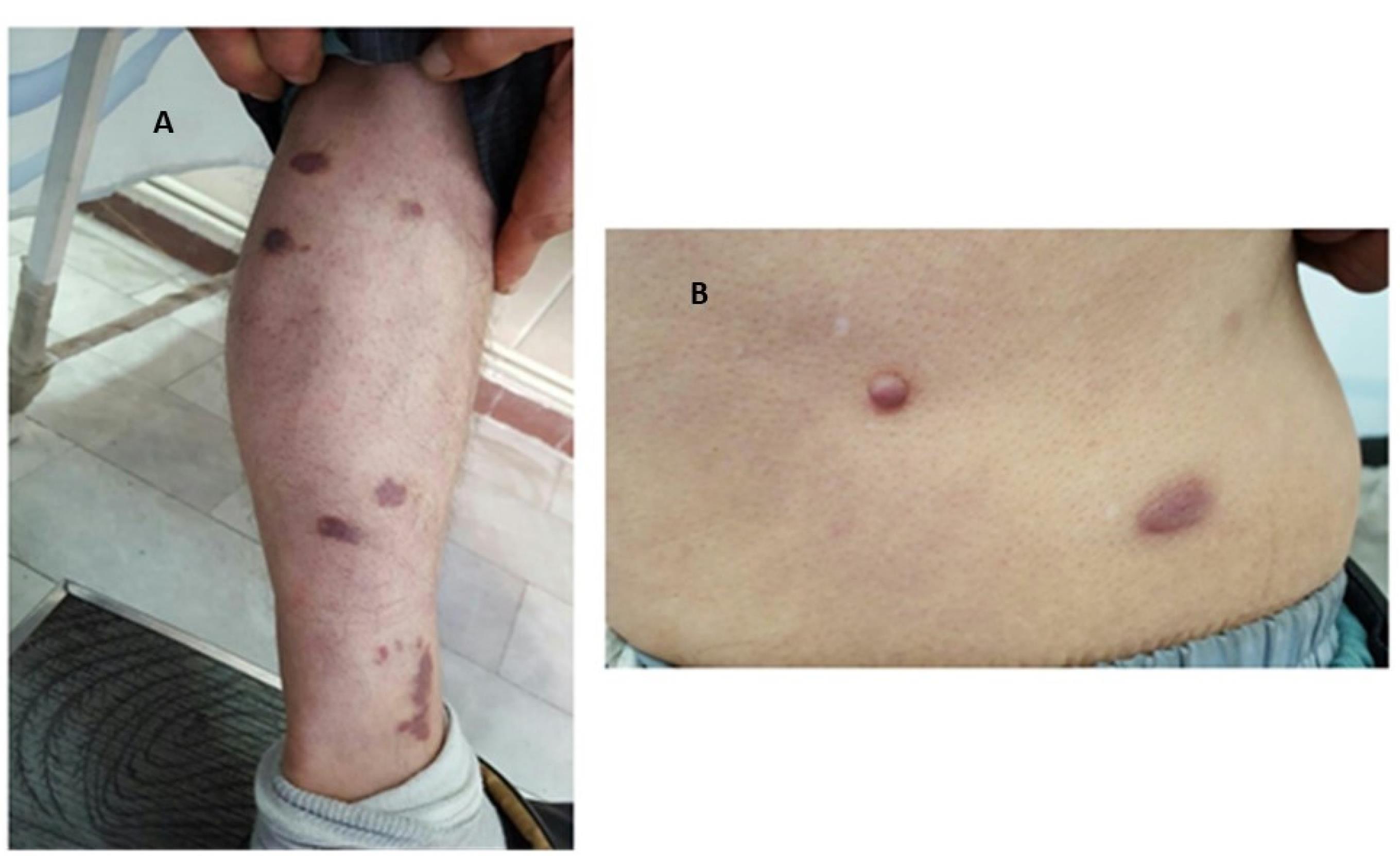
Figure 1.
Well demarcated violaceous to brown plaques on the lower extremities and trunk.
.
Well demarcated violaceous to brown plaques on the lower extremities and trunk.
No edema was observed on the lower extremities. There were also multiple red and purple plaques and nodules on the neck, lower face, nose, and ears (Figure 2A). Interestingly, there was a painless fleshy nodule with a size of 1.5 × 1.5 in his upper gingiva (Figure 2B).

Figure 2.
(A) Violaceous to erythematous patches and plaques, involving the face and neck, a common site in AIDS‐associated KS. (B) Asymptomatic Purple nodule in the gingiva, a less common presentation of classic KS (scale 40×).
.
(A) Violaceous to erythematous patches and plaques, involving the face and neck, a common site in AIDS‐associated KS. (B) Asymptomatic Purple nodule in the gingiva, a less common presentation of classic KS (scale 40×).
Erythematous plaques on the face and neck are common signs of AIDS-associated KS. Biopsy of the skin lesion showed angiomatous proliferation of small vessels and slits with mild perivascular lymphocytic infiltration containing plasma cell and red blood cell (RBC) extravasation in the dermis (Figure 3A). Both the complete blood count (CBC) test and chest X ray were normal. HIV test was negative twice and CD4 count was in normal range. The staining results showed strong immune reactivity of all neoplastic cells to CD31 and CD34 (Figure 3B).
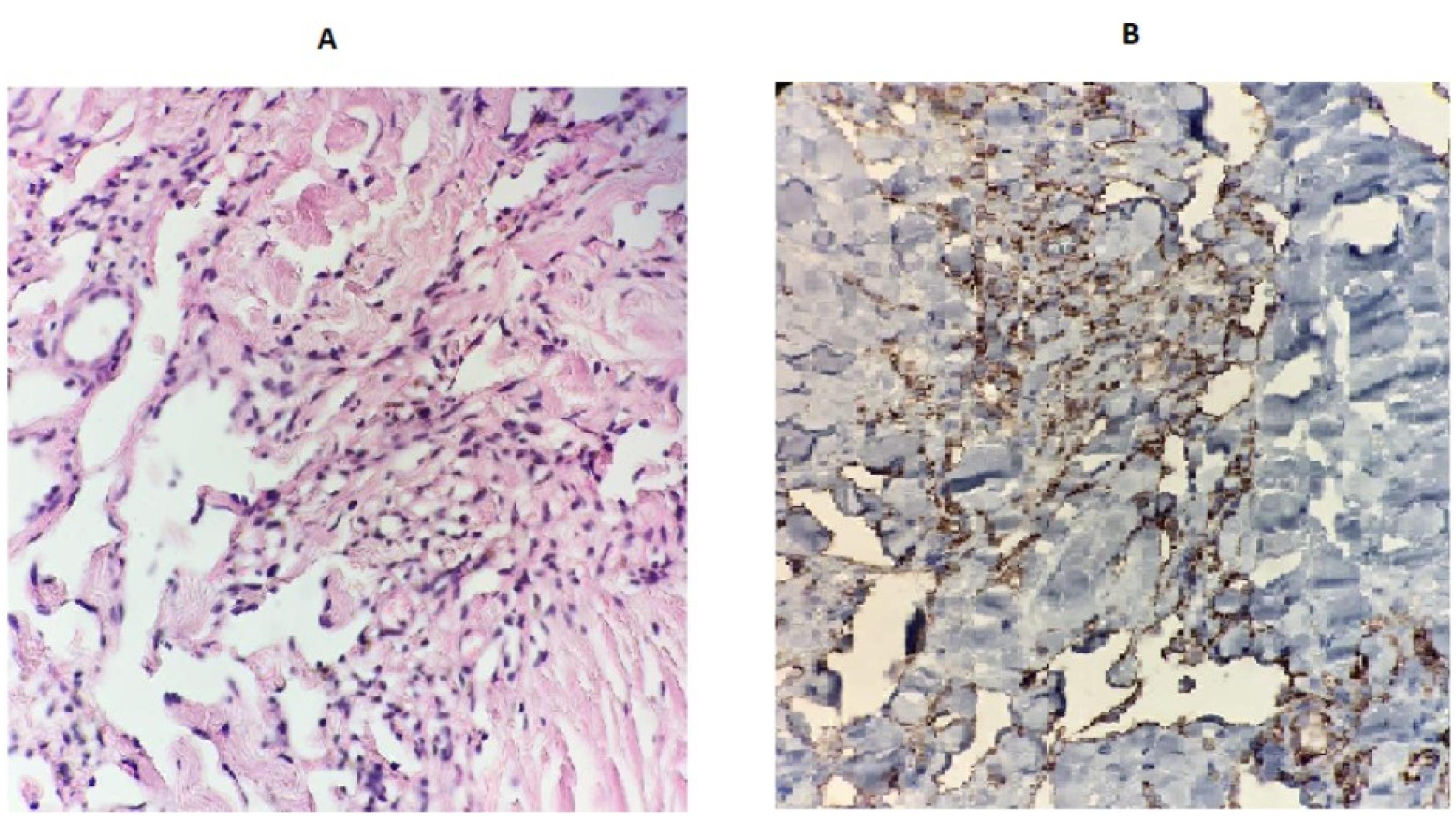
Figure 3.
(A) Positive irregular dilated vascular channels associated with hemosiderin deposition and focal inflammation. (B) Immunohistochemistry for the vascular marker CD31
.
(A) Positive irregular dilated vascular channels associated with hemosiderin deposition and focal inflammation. (B) Immunohistochemistry for the vascular marker CD31
Blood test analyses using PCR showed that HHV-8 was positive. Treatment of the patient was started with doxorubicin and paclitaxel (dose of 340-380 mg/m2), leading to improvement in his outcomes.
Discussion
KS is a vascular neoplasm which usually has a multifocal origin, with multiple vascular nodules on the skin and other organs. It also involves lymph nodes and visceral organs, especially the respiratory and gastrointestinal tracts.20 Primary classic KS of the head and neck is rare in any case. Ben et al reported a 71-year-old immunocompetent man who presented with a three-month history of a slowly progressive swelling in the right parotid region. They discussed the peculiarity of the presentation, the differential diagnosis, and the management strategy of such a rare disease.21 A study carried out by Ascoli et al on a 57-year-old white female patient of Greek origin showed that non-HIV-related KS is an HHV-8-related KS, an angioproliferative skin cancer that can cause pain, disfigurement, and limb dysfunction.22 In the present study, we report the case of a 66-years-old man with progressive skin lesions, including purple patches with multiple deep plaques and red to brown nodules disseminated all over the body and oral mucosa. Although no definitive regimen was established, we started with doxorubicin and paclitaxel and shrinkage of lesions was obvious after two sessions. It would be beneficial to investigate the effectiveness of currently-available treatments in these patients. It can be concluded that non-HIV-related KS can have the same signs as HIV-related KS.
Competing Interests
None to be declared.
Authors’ Contribution
Conceptualization: Mahsa Eslami.
Data curation: Sanaz Alizadeh.
Formal analysis: Faezeh Alavi.
Funding acquisition: Sina Safari.
Investigation: Sina Safari.
Methodology: Mahsa Eslami.
Resources: Faezeh Alavi.
Supervision: Sina Sfari.
Writing–original draft: Faezeh Alavi.
Writing–review & editing: Sanaz Alizadeh.
Ethical Approval
Informed consent was obtained form the patient for publication of this report.
References
- Trujillo JM, de Magalhães Alves NR, Medeiros PM, Azulay-Abulafia L, de Fátima Guimarães Scotelaro Alves M, Gripp AC. Clinical exuberance of classic Kaposi’s sarcoma and response to radiotherapy. An Bras Dermatol 2015; 90(6):883-6. doi: 10.1590/abd1806-4841.20153877 [Crossref] [ Google Scholar]
- Phavixay L, Raynolds D, Simman R. Non AIDS Kaposi’s sarcoma leading to lower extremities wounds, case presentations and discussion. J Am Coll Clin Wound Spec 2012; 4(1):13-5. doi: 10.1016/j.jccw.2013.01.003 [Crossref] [ Google Scholar]
- Attwa E, Gharib K, Albalat W, Amer A. Classical Kaposi sarcoma: case reports with unusual presentation on the penis and scrotum. Int J Dermatol 2016; 55(10):e533-8. doi: 10.1111/ijd.13319 [Crossref] [ Google Scholar]
- Gilani JA, Ullah Khan A, Shahid S, Ullah Khan I, Ullah Khan S. Clinical presentation of non-HIV Kaposi sarcoma. J Coll Physicians Surg Pak 2009; 19(9):586-8. [ Google Scholar]
- Kodra A, Walczyszyn M, Grossman C, Zapata D, Rambhatla T, Mina B. Case report: pulmonary Kaposi sarcoma in a non-HIV patient. F1000Res 2015; 4:1013. doi: 10.12688/f1000research.7137.1 [Crossref] [ Google Scholar]
- Jan RA, Koul PA, Ahmed M, Shah S, Mufti SA, War FA. Kaposi sarcoma in a non HIV patient. Int J Health Sci (Qassim) 2008; 2(2):153-6. [ Google Scholar]
- Hiatt KM, Nelson AM, Lichy JH, Fanburg-Smith JC. Classic Kaposi sarcoma in the United States over the last two decades: a clinicopathologic and molecular study of 438 non-HIV-related Kaposi sarcoma patients with comparison to HIV-related Kaposi sarcoma. Mod Pathol 2008; 21(5):572-82. doi: 10.1038/modpathol.2008.15 [Crossref] [ Google Scholar]
- Simonart T. Non-HIV-related Kaposi’s sarcoma in former colonists/expatriates in Central Africa. J Travel Med 2009; 16(2):134-5. doi: 10.1111/j.1708-8305.2008.00289.x [Crossref] [ Google Scholar]
- Galleu A, Fozza C, Simula MP, Contini S, Virdis P, Corda G. CD4 + and CD8 + T-cell skewness in classic Kaposi sarcoma. Neoplasia 2012; 14(6):487-94. doi: 10.1596/neo.11646 [Crossref] [ Google Scholar]
- Fonseca Aizpuru EM, Arias Miranda I, García-Alcalde ML, Nuño Mateo FJ. [A 28 year-old woman non-HIV with Kaposi’s sarcoma, thrombocytopenic purpura and hypogammaglobulinemia]. An Med Interna 2008; 25(2):100. doi: 10.4321/s0212-71992008000200013.[Spanish] [Crossref] [ Google Scholar]
- Gill K, Shah J. Kaposi sarcoma in patients with diabetes and wounds. Adv Skin Wound Care 2006; 19(4):198-201. [ Google Scholar]
- Wani GM, Ahmad SM, Qayoom S, Khursheed B, Khan AR. Corticosteroid induced, HHV-8 positive Kaposi’s sarcoma in a non-HIV elderly patient. J IMA 2012; 44(1):44-1. doi: 10.5915/44-1-9317 [Crossref] [ Google Scholar]
- Sen F, Tambas M, Ciftci R, Toz B, Kilic L, Bozbey HU. Factors affecting progression-free survival in non-HIV-related Kaposi sarcoma. J Dermatolog Treat 2016; 27(3):275-7. doi: 10.3109/09546634.2015.1094177 [Crossref] [ Google Scholar]
- Yang H, Lu QL, Wu XJ, Ma HY, Qu YY, Zhang DZ. Association of genetic variations in miR-146a rs2910164 and miR-149 rs11614913 with the development of classic Kaposi sarcoma. Genet Mol Res 2016; 15(4):gmr15048855. doi: 10.4238/gmr15048855 [Crossref] [ Google Scholar]
- Que SK, DeFelice T, Abdulla FR, Cassarino D, Patel RR. Non-HIV-related Kaposi sarcoma in 2 Hispanic patients arising in the setting of chronic venous insufficiency. Cutis 2015; 95(6):E30-3. [ Google Scholar]
- Parakh S, Goh M, Andrews MC. Non-HIV-associated Kaposi sarcoma in an immunosuppressed melanoma patient treated with dabrafenib. J Clin Pharm Ther 2016; 41(3):354-6. doi: 10.1111/jcpt.12366 [Crossref] [ Google Scholar]
- Akasbi Y, Awada A, Arifi S, Mellas N, El Mesbahi O. Non-HIV Kaposi’s sarcoma: a review and therapeutic perspectives. Bull Cancer 2012; 99(10):92-9. doi: 10.1684/bdc.2012.1636 [Crossref] [ Google Scholar]
- Vincenzi B, D’Onofrio L, Frezza AM, Grasso RF, Fausti V, Santini D. Classic Kaposi sarcoma: to treat or not to treat?. BMC Res Notes 2015; 8:138. doi: 10.1186/s13104-015-1076-1 [Crossref] [ Google Scholar]
- Schmidt BM, Holmes CM. Classic solitary Kaposi sarcoma of the foot in an immunocompetent patient: a case report. Wounds 2016; 28(9):E35-E40. [ Google Scholar]
- Yun JJ, Preda V, Frankum B. Chronic human herpes virus 8 infection successfully treated with valganciclovir. World Allergy Organ J 2009; 2(7):128-9. doi: 10.1097/WOX.0b013e3181abe7b6 [Crossref] [ Google Scholar]
- Ben M’barek L, Fardet L, Mebazaa A, Thervet E, Biet I, Kérob D. A retrospective analysis of thalidomide therapy in non-HIV-related Kaposi’s sarcoma. Dermatology 2007; 215(3):202-5. doi: 10.1159/000106576 [Crossref] [ Google Scholar]
- Ascoli V, Minelli G, Kanieff M, Crialesi R, Frova L, Conti S. Cause-specific mortality in classic Kaposi’s sarcoma: a population-based study in Italy (1995-2002). Br J Cancer 2009; 101(7):1085-90. doi: 10.1038/sj.bjc.6605265 [Crossref] [ Google Scholar]