Dr. Akbar Rahmani is a boardcertified internist specializing in endocrinology. As such, he is experienced in diagnosing and treating conditions related to the endocrine system, including diabetes, thyroid diseases, and
metabolic disorders. He has over thirty years of experience practicing in the south suburbs as a member of
Ingalls Medical Staff. He graduated from University of Tabriz Medical School and he attendant to internship in Advocate Christ Hospital. He passed his residency and fellow in Rush Presbyterian St. Lukes Medical Center; Advocate Christ Medical Center and John H Stroger Hospital of Cook County more than 20 years ago.
Copyright and License Information
© 2023 The Author(s).
This is an open-access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Introduction
Diabetes, sometimes referred to as diabetes mellitus, is a collective term for a range of illnesses that impact how the body utilizes glucose, or blood sugar. First of all, glucose is an essential source of energy for the cells that comprise muscles and tissues. It is also the primary energy source for the brain. Diabetes has several primary causes. However, regardless of the type of diabetes the patient may suffer from, this illness may result in an excess of sugar in the blood. A blood sugar level that is extremely high might cause major health issues. Type 1 and type 2 diabetes are chronic diabetes diseases. Prediabetes and gestational diabetes are two diabetes disorders that may be treated.1,2 Prediabetes develops when blood sugar levels are higher than usual. However, the blood sugar is not elevated enough to qualify as diabetes. Furthermore, if preventative measures are not implemented, prediabetes might progress to diabetes. Gestational diabetes develops throughout pregnancy. However, when the baby is delivered, it can disappear. One early and crucial stage in the development of vascular problems is the adherence of leucocytes to endothelial cells. These molecules use a series of sequential processes regulated by certain adhesion molecules on leucocytes and endothelial cells to mediate inflammation, endothelial dysfunction, and the development of micro and macrovascular problems.3 Diabetes may be due to a variety of causes related to cell adhesion proteins. The most significant of them include selectins, integrins, and cell adhesion molecules such as intercellular adhesion molecules (ICAM) and vascular cell adhesion molecules. Transmembrane receptors called integrins facilitate adhesion between cells and between cells and the extracellular matrix (ECM).4 Integrins mediate cellular signals, including the control of the cell cycle, the arrangement of the intracellular cytoskeleton, and the translocation of novel receptors to the cell membrane, by activating signal transduction pathways upon ligand interaction. Integrins provide quick and adaptable reactions to stimuli occurring at the cell surface. According to the findings, diabetes is caused by an overexpression of Integrin.5 According to recent research, integrins serve as transmembrane linkers, or “integrators”, mediating the connections between the ECM and the cytoskeleton that are necessary for cells to adhere to the matrix.3,6 Integrins bind to ligands and then trigger signal transduction pathways that mediate many physiological signals, including the migration of new receptors to the cell membrane, control of the cell cycle, and organization of the intracellular cytoskeleton.5 ICAM-1 belongs to the immunoglobulin superfamily, which is a protein class that also includes T-cell receptors and antibodies. ICAM-1 is a transmembrane protein with a single transmembrane domain, a carboxy-terminus cytoplasmic domain, and an amino-terminus extracellular domain.6 It has a structure that is heavily glycosylated, and its extracellular domain is made up of many loops that are formed by disulfide bridges within the protein (Figure 1). Considering that the beta sheet is the protein’s predominant secondary structure, scientists have theorized that ICAM-1 contains dimerization domains. ICAM-1 is a biomarker for diabetic nephropathy prognosis.7 One of the various routes that ICAM-1 is engaged in is the anti-inflammatory one. Experiments have shown that ICAM-1 gene expression suppression may slow the progression of diabetes and DN, notwithstanding the complexity of the picture surrounding ICAM-1 participation and interaction. In addition to increasing the release of insulin from pancreatic islets, glucagon-like peptide-1 has a number of extra-pancreatic effects. Syndecan-4 is a type I transmembrane proteoglycan containing heparan sulfate that serves as an intracellular signaling receptor. The protein belongs to the syndecan proteoglycan family and is found as a homodimer. Growth factors, anticoagulants, and ECM are all interacting with syndecan-4. It also controls cell adhesion, migration, and the actin cytoskeleton. Protein kinase C (PKC), an enzyme involved in signal transduction, is activated by syndecan-4.3,8 It is possible that the syndecan-4 variable domain functions as a self-association site. Considering that kinase activity and syndecan-4 clustering are correlated, PKC activity and syndecan-4 clustering are correlated as well. Additionally, syndecan-4 boosts PKC activity tenfold by binding to phosphatidylinositol 4-bisphosphate via the variable domain. Specifically, keratinocytes obtained from diabetic patients migrate more readily when exposed to syndecan-4 proteoliposomes. Furthermore, syndecan-4 proteoliposomes increase the intracellular signaling response to platelet-derived growth factor-BB (PDGF-BB) by sensitizing keratinocytes to PDGF-BB stimulation.5,9
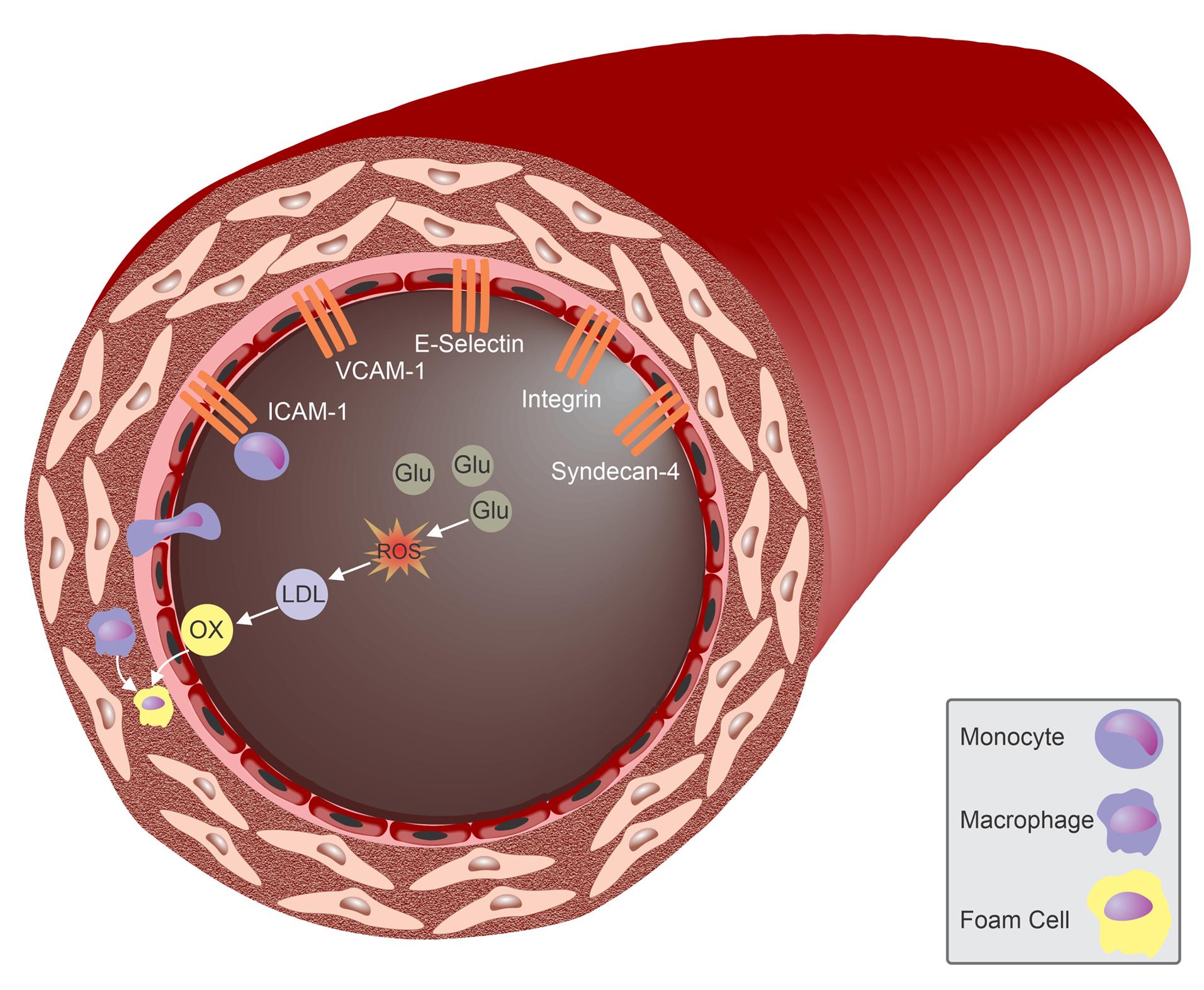
Figure 1.
Role of Cell Adhesion Proteins in Diabetes
.
Role of Cell Adhesion Proteins in Diabetes
Acknowledgements
I would like to appreciate the cooperation of UChicago Medicine Medical Group.
Competing Interests
The author declares that he has no competing interests.
Consent for Publication
Not applicable.
Ethical Approval
Not applicable.
Funding
None.
References
- Falcão VT, Maschio DA, de Fontes CC, Oliveira RB, Santos-Silva JC, Almeida AC. Reduced insulin secretion function is associated with pancreatic islet redistribution of cell adhesion molecules (CAMS) in diabetic mice after prolonged high-fat diet. Histochem Cell Biol 2016; 146(1):13-31. doi: 10.1007/s00418-016-1428-5 [Crossref] [ Google Scholar]
- Goldberg RB. Cytokine and cytokine-like inflammation markers, endothelial dysfunction, and imbalanced coagulation in development of diabetes and its complications. J Clin Endocrinol Metab 2009; 94(9):3171-82. doi: 10.1210/jc.2008-2534 [Crossref] [ Google Scholar]
- Grossin N, Wautier MP, Wautier JL. Red blood cell adhesion in diabetes mellitus is mediated by advanced glycation end product receptor and is modulated by nitric oxide. Biorheology 2009; 46(1):63-72. doi: 10.3233/bir-2009-0519 [Crossref] [ Google Scholar]
- Milne R, Brownstein S. Advanced glycation end products and diabetic retinopathy. Amino Acids 2013; 44(6):1397-407. doi: 10.1007/s00726-011-1071-3 [Crossref] [ Google Scholar]
- Nomura S, Shouzu A, Omoto S, Inami N, Tanaka A, Nanba M. Correlation between adiponectin and reduction of cell adhesion molecules after pitavastatin treatment in hyperlipidemic patients with type 2 diabetes mellitus. Thromb Res 2008; 122(1):39-45. doi: 10.1016/j.thromres.2007.08.013 [Crossref] [ Google Scholar]
- Nowak M, Wielkoszyński T, Marek B, Kos-Kudła B, Swietochowska E, Siemińska L. Blood serum levels of vascular cell adhesion molecule (sVCAM-1), intercellular adhesion molecule (sICAM-1) and endothelial leucocyte adhesion molecule-1 (ELAM-1) in diabetic retinopathy. Clin Exp Med 2008; 8(3):159-64. doi: 10.1007/s10238-008-0173-z [Crossref] [ Google Scholar]
- Okada S, Shikata K, Matsuda M, Ogawa D, Usui H, Kido Y. Intercellular adhesion molecule-1-deficient mice are resistant against renal injury after induction of diabetes. Diabetes 2003; 52(10):2586-93. doi: 10.2337/diabetes.52.10.2586 [Crossref] [ Google Scholar]
- Otsuki M, Hashimoto K, Morimoto Y, Kishimoto T, Kasayama S. Circulating vascular cell adhesion molecule-1 (VCAM-1) in atherosclerotic NIDDM patients. Diabetes 1997; 46(12):2096-101. doi: 10.2337/diab.46.12.2096 [Crossref] [ Google Scholar]
- Schmidt AM, Hori O, Chen JX, Li JF, Crandall J, Zhang J. Advanced glycation endproducts interacting with their endothelial receptor induce expression of vascular cell adhesion molecule-1 (VCAM-1) in cultured human endothelial cells and in mice A potential mechanism for the accelerated vasculopathy of diabetes. J Clin Invest 1995; 96(3):1395-403. doi: 10.1172/jci118175 [Crossref] [ Google Scholar]